NR509 Week 6 iHuman Case Bebe Babbit
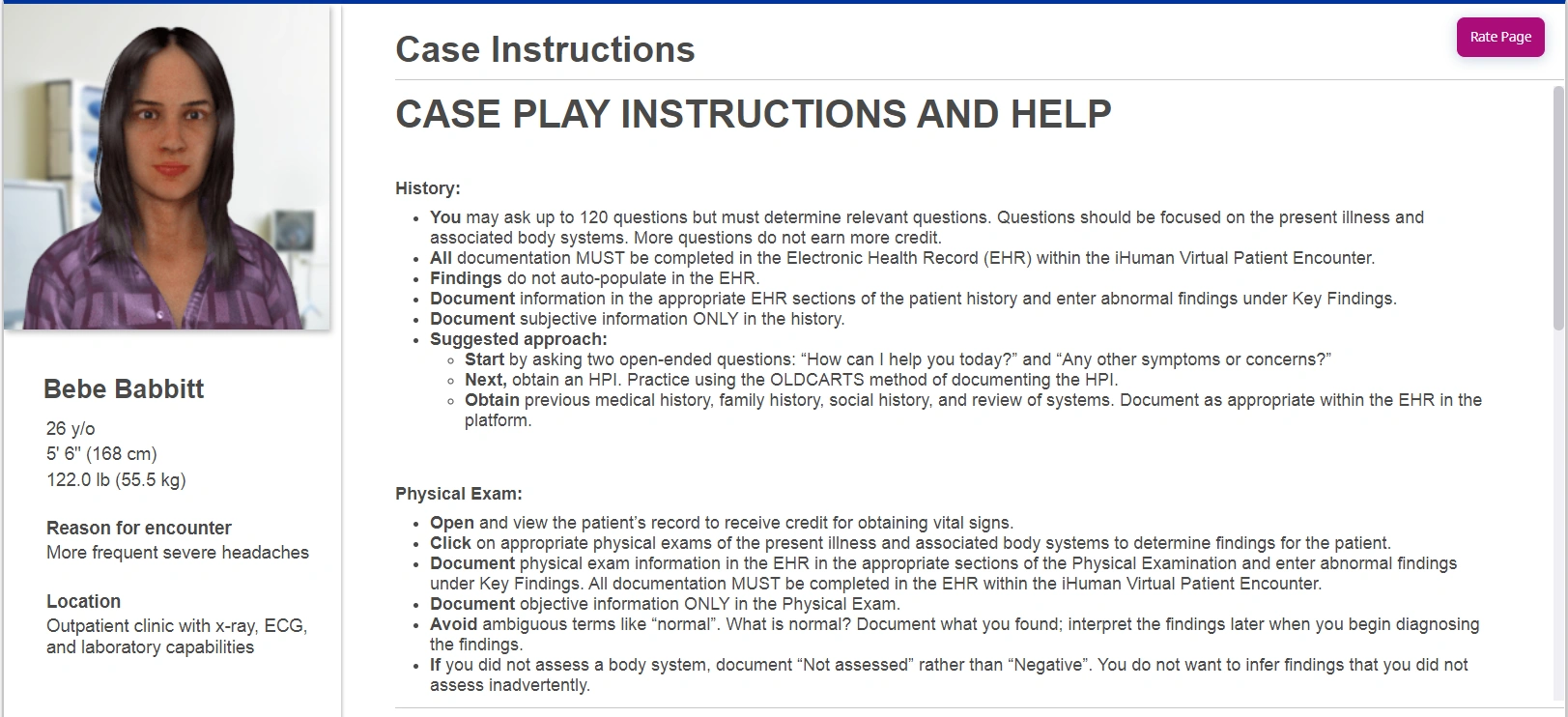
Case Instructions (Bebe Babbitt)
History:
-
You may ask up to 120 questions but must determine relevant questions. Questions should be focused on the present illness and associated body systems. More questions do not earn more credit.
-
All documentation MUST be completed in the Electronic Health Record (EHR) within the iHuman Virtual Patient Encounter.
-
Findings do not auto-populate in the EHR.
-
Document information in the appropriate EHR sections of the patient history and enter abnormal findings under Key Findings.
-
Document subjective information ONLY in the history.
Suggested Approach:
-
Start by asking two open-ended questions:
-
“How can I help you today?”
-
“Any other symptoms or concerns?”
-
-
Next, obtain an HPI. Practice using the OLDCARTS method of documenting the HPI.
-
Obtain previous medical history, family history, social history, and review of systems. Document as appropriate within the EHR in the platform.
Patient Info:
-
Name: Bebe Babbitt
-
Age: 26 y/o
-
Height: 5’6” (168 cm)
-
Weight: 122 lbs (55.5 kg)
-
Reason for Encounter: More frequent severe headaches
-
Location: Outpatient clinic with x-ray, ECG, and laboratory capabilities
Physical Exam:
-
Open and view the patient’s record to receive credit for obtaining vital signs.
-
Click on appropriate physical exams of the present illness and associated body systems to determine findings.
-
Document physical exam information in the EHR and enter abnormal findings under Key Findings.
-
Document objective information ONLY in the Physical Exam.
-
Avoid ambiguous terms like “normal.” Document exactly what you found.
-
If you did not assess a body system, document “Not assessed” rather than “Negative.”
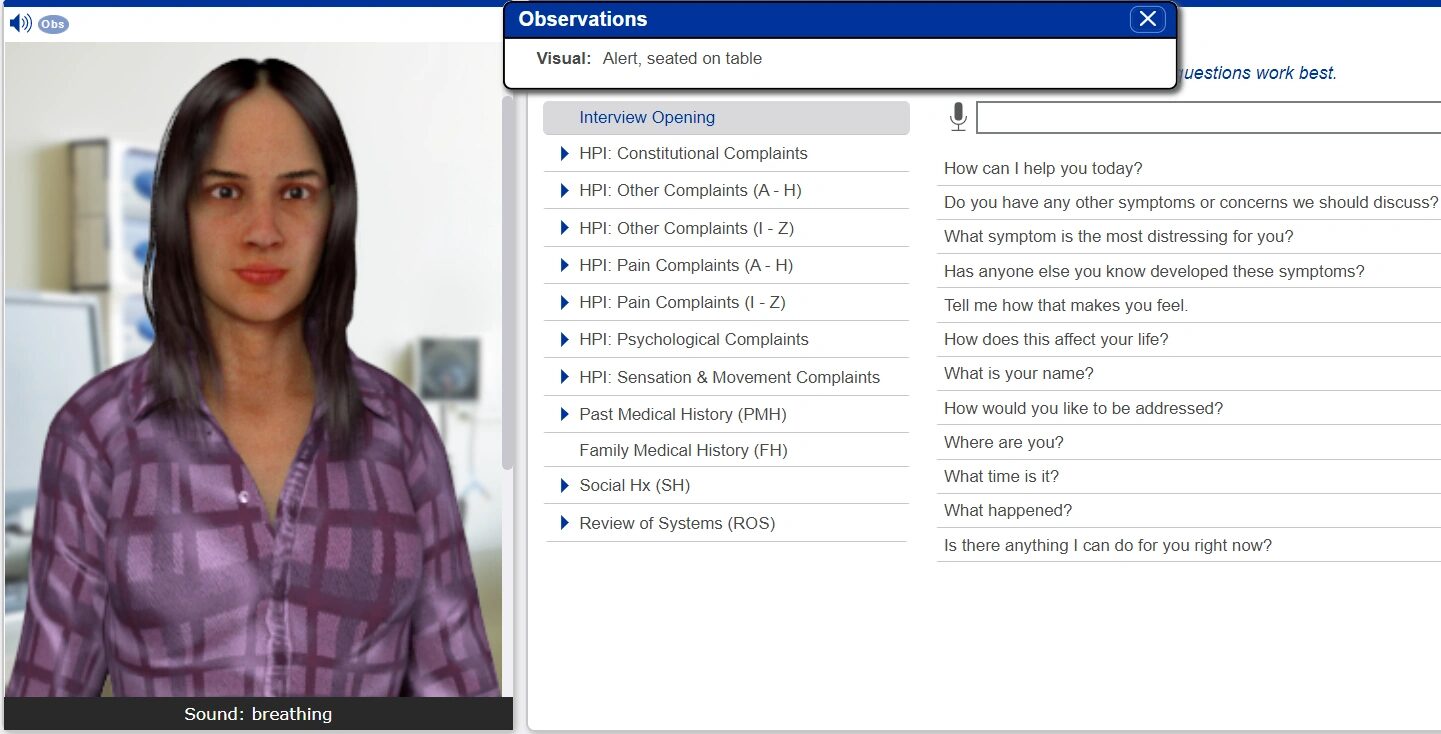
Observation (Virtual Encounter)
-
Visual: Alert, seated on table
-
Sound: Breathing
Interview Opening Sample Questions:
-
How can I help you today?
-
Do you have any other symptoms or concerns we should discuss?
-
What symptom is the most distressing for you?
-
Has anyone else you know developed these symptoms?
-
Tell me how that makes you feel.
-
How does this affect your life?
-
What happened?
-
Is there anything I can do for you right now?
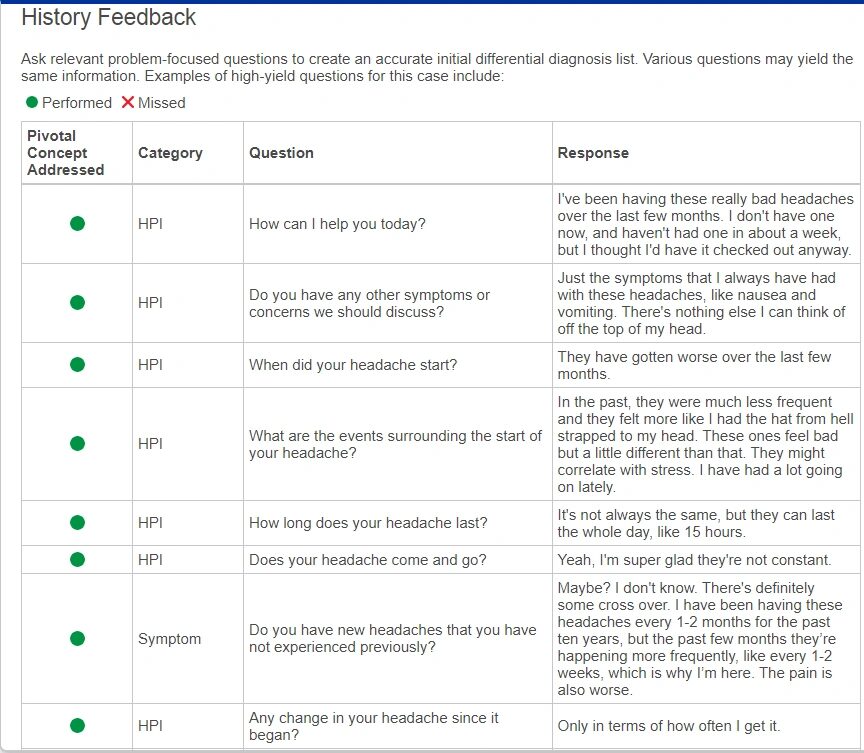
History Feedback (High-Yield Questions & Responses)
-
How can I help you today?
“I’ve been having these really bad headaches over the last few months. I don’t have one now, but I thought I’d get it checked out.” -
Other symptoms?
“Just nausea and vomiting with headaches.” -
When did your headache start?
“They’ve gotten worse over the last few months.” -
Events surrounding start?
“In the past they were less frequent. These feel worse and may correlate with stress.” -
How long do they last?
“Sometimes 15 hours.” -
Do they come and go?
“Yes, not constant.” -
New headaches?
“Yes, more frequent now (every 1–2 weeks vs. every 1–2 months).” -
Changes?
“Only in terms of frequency.”
Detailed Symptom & History Notes
-
Headache location: Left, behind eye
-
Radiation: No, stays behind left eye
-
Aura: Spotty vision, zig-zag flashing lights before onset
-
Character: Throbbing, pulsating, very unpleasant
-
Severity: Starts 2–3/10, progresses to 8–10/10, lasts up to 15 hrs
-
Relieving factors: Sleep, dark quiet room
-
Aggravating factors: Light and noise
-
Treatment history: Tried acetaminophen/ibuprofen, but ineffective now due to nausea
-
Nausea/vomiting: Yes, with bad headaches only
-
Past history: Headaches for 10 years, no major trauma or surgeries except dental fillings
-
Meds: Uses Benadryl during finals, OTC acetaminophen/ibuprofen as per box, not effective now
-
Allergies: None known
-
Family history: Not available (no siblings, limited parental info)
Reviews
There are no reviews yet.